
(Photo by Karola G via Pexels)
By Stephen Beech
Many sexual assault victims also suffer a form of brain damage, reveals new research.
Previous studies have shown that around 70% of women develop post-traumatic stress disorder (PTSD) after being attacked.
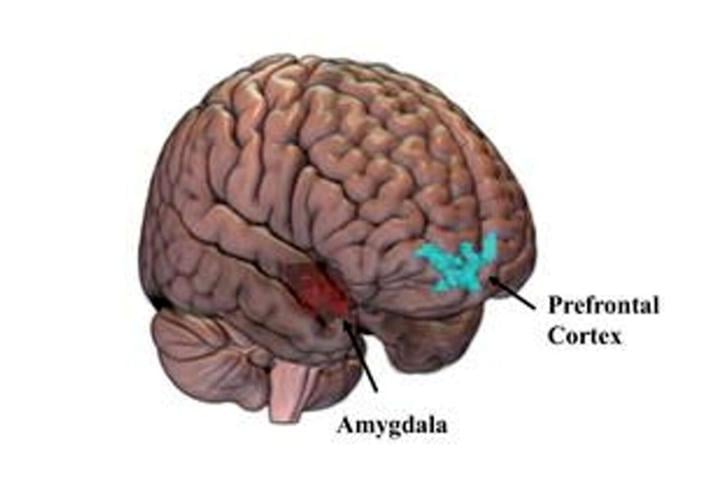
Now scientists have shown that many of those women show a "marked reduction" in the usual communication between the amygdala and the pre-frontal cortex - two important brain areas involved in processing and control of emotions.
Synchronization between the two areas can drop to near zero in some women sex attack victims, according to the findings.
Previous PTSD studies, after natural disasters, accidents or war, have revealed changes in how the brain communicates.
Now a team of Spanish scientists have shown that sexual assault can lead to similar brain changes.

(Photo by Pixabay via Pexels)
The researchers studied 40 women with PTSD as a result oft sexual assault trauma within the past year, recruited from the Hospital Clinic of Barcelona, along with a matched control group.
All the participants underwent brain scans to look at connectivity, and how they relate to depressive and PTSD symptoms.
Lead researcher Dr. Lydia Fortea, of the Hospital Clinic, Barcelona, said: “PTSD following sexual assault tends to be especially severe and is often accompanied by higher rates of depression, anxiety, and suicidal thoughts.
"Despite sexual violence being one of the most widespread forms of trauma affecting women, most research on PTSD has focused on other types of trauma, such as war."
She says the study is one of the first, and the largest, to look at PTSD in sexual assault in teenagers and adult women.

(Photo by Liza Summer via Pexels)
Dr. Fortea said: "We looked at how key brain regions involved in fear and emotion regulation synchronize with the rest of the brain in women with PTSD following sexual assault.
"We focused on the fronto-limbic system, which plays a crucial role in regulating emotions and responding to threats.
"We found that in 22 of the 40 women with PTSD following a recent sexual assault, communication between the amygdala and the prefrontal cortex was effectively lost, dropping to zero or near zero.
"The amygdala helps process emotions like fear, and the prefrontal cortex, helps control and regulate those emotions.
"When this connection weakens, the brain might struggle to manage fear responses or regulate emotions, which could explain why people with PTSD often experience intense fear and mood changes.

Location of amygdala and prefrontal cortex in the brain. (Lydia Fortew via SWNS)
"However, we didn’t find that this brain change was directly linked to how severe their PTSD and depressive symptoms were.
"This suggests that while this brain difference might be a feature of the disorder itself, it’s not necessarily a sign of how bad the symptoms are; this is probably dependent on other factors."
She added: "This supports the idea that PTSD after sexual assault is linked to problems in brain circuits that regulate emotion and fear.
"One of the things we will do now is to see if these connectivity disruptions following a sexual assault could help to predict response to PTSD treatment.
"If so, we would be able to identify early which patients are at risk of worse outcomes and intensify clinical efforts to help them recover.
"So far, this is a study of 40 women, but the work is ongoing.
We need more studies to confirm the findings”.

(Photo by Vika Yagupa via Pexels)
The findings were presented at the European College of Neuropsychopharmacology (ECNP) conference in Amsterdam.
Professor Marin JukiÄ, of the University of Belgrade, Serbia, says the findings could improve care for victims of sexual assault.
JukiÄ, who was not involved in the work, said: “This study demonstrates profound fronto-limbic dysconnectivity in women with PTSD following sexual assault, a population historically underrepresented in brain connectivity research.
"The finding that amygdala–prefrontal communication can drop to near zero underscores the severity of circuit-level disruptions in emotional regulation networks after trauma.
"Notably, the absence of a direct correlation with symptom severity suggests that these connectivity deficits may serve more as a biological signature of the disorder rather than a state-dependent marker."
He added: "This raises the possibility that such disruptions could become predictive biomarkers for treatment response, guiding personalised interventions.
"However, larger studies are needed to determine how these neural patterns evolve and whether targeted therapies can ameliorate connectivity."
























(0) comments
Welcome to the discussion.
Log In
Keep it Clean. Please avoid obscene, vulgar, lewd, racist or sexually-oriented language.
PLEASE TURN OFF YOUR CAPS LOCK.
Don't Threaten. Threats of harming another person will not be tolerated.
Be Truthful. Don't knowingly lie about anyone or anything.
Be Nice. No racism, sexism or any sort of -ism that is degrading to another person.
Be Proactive. Use the 'Report' link on each comment to let us know of abusive posts.
Share with Us. We'd love to hear eyewitness accounts, the history behind an article.